Cervical cancer, once a silent adversary lurking behind vague symptoms, has, in the era of advanced medical science, become a condition whose trajectory can be mapped with far greater precision. Prognosis today is no longer a matter of guesswork but a confluence of clinical insight, diagnostic sharpness, and individualized treatment pathways. For patients traveling across borders in pursuit of high-standard oncologic care, understanding survival rates and long-term outcomes is pivotal not only for medical decision-making but also for regaining emotional equilibrium during an undeniably turbulent chapter.
This detailed guide explores the prognosis, survival rates, recurrence patterns, reproductive concerns, and quality-of-life considerations for women diagnosed with cervical cancer. It synthesizes global oncologic protocols, contemporary clinical evidence, and experiential observations commonly reported within medical tourism programs.
Understanding Factors That Shape Cervical Cancer Prognosis
Cervical cancer does not behave in a monolithic fashion; instead, it behaves more like a mosaic, its aggressiveness, spread, and treatment responsiveness shaped by a series of interlocking variables. Doctors typically assess the following elements before forecasting a woman’s survival outlook:
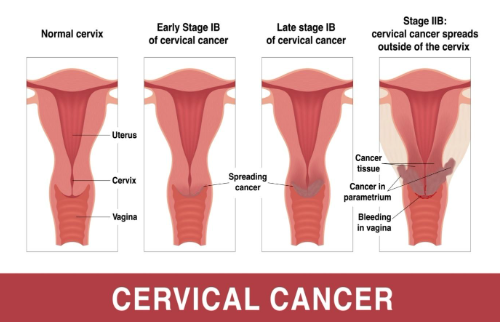
The Stage of the Disease The single most potent determinant of prognosis is the stage at which the cancer is diagnosed.
- Early-stage disease confined to the cervix has remarkably high survival rates when managed according to international oncology standards. It has the highest cure rates, often achieved through surgery alone or minimal adjuvant therapy.
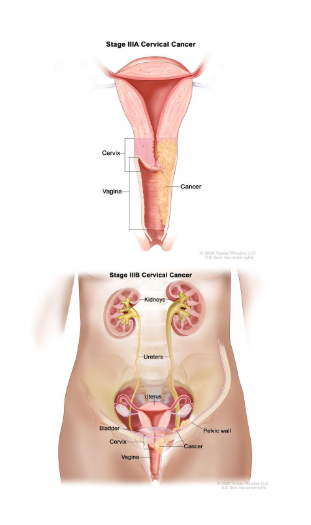
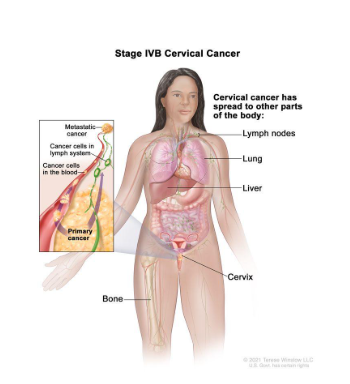
- Advanced-stage disease (stage 2-4), on the other hand, often signals deeper tissue infiltration or distant organ involvement, making treatment more challenging. The spread of cancer ranges from infiltrating the surrounding pelvic tissue (stage 2), extending to the pelvic side wall or affecting the kidneys (stage 3), and may spread to distant organs (stage 4). Treatment in these stages becomes multi-modality, and the outlook is more guarded.
Location of the Malignancy inside the Cervix Some tumors sit near the external part of the cervix, while others implant deeper into the endocervical canal. Their position affects both the type of symptoms they cause and the complexity of the surgery required.
Histological Type of Cervical Cancer While the treatment protocol overlaps, the cell type influences detection and behavior. Most cases fall into one of two primary categories:
- Squamous cell carcinoma (by far the most common): Accounts for about 80% of the cases. It arises from flat, surface cells of the ectocervix. SCC is typically easier to detect early via a routine Pap smear as it develops on the accessible outer portion of the cervix.
- Adenocarcinoma (arising from glandular tissue): accounts for about 15-20% of cases. It originates from glandular cells deep in the endocervical canal. This location makes it harder to sample accurately during a Pap smear, and it occasionally exhibits more aggressive behavior, which can lead to delayed detection and impact outcomes.
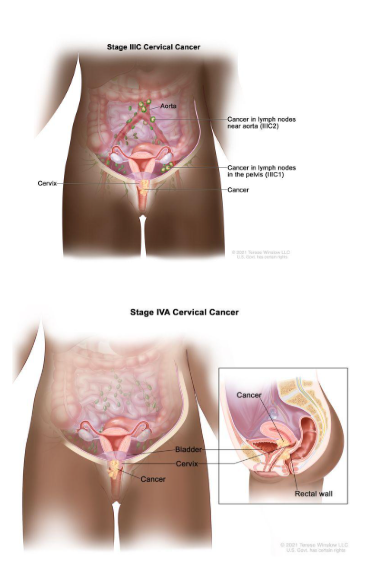
Presence of Lymph Node Metastasis Cervical cancer often spreads through lymphatic pathways. The moment malignant cells lodge in pelvic or para-aortic lymph nodes, the prognosis shifts. The number of affected nodes serves as a foreboding marker; each additional node involved diminishes survival percentages. Nodal involvement is categorized by:
- Location: Pelvic nodes versus more ominous para-aortic nodes; the latter are a major point for systemic spread.
- Number: The volume of disease, specifically the number of affected nodes, is a critical prognostic criterion.
Depth of Tumor Invasion (parametrial and vascular involvement) A localized tumor behaves differently from one that has infiltrated the parametrial tissues (fibrous tissue next to the uterus), uterine structures, or pelvic side walls. Tumors breaking past these boundaries typically require multi-modality treatment, including combinations of surgery, radiation, and chemotherapy. Similarly, the presence of cancer cells in the small blood and lymphatic vessels (lymph vascular space invasion or LVSI) is a sign of aggressive biological cancer and requires closer surveillance or adjuvant therapy.
Collectively, these factors act like coordinates on an oncologist’s navigational chart, helping guide treatment strategies and expected recovery trajectories.
Survival Outcomes after Radical Hysterectomy in Early-Stage Disease
For many women diagnosed with Stage I or II cervical cancer, radical hysterectomy remains a cornerstone curative procedure. This surgery involves the removal of the uterus, cervix, tissues surrounding the cervix (parametrium), and a portion of the upper vagina. Pelvic lymph node dissection is often performed simultaneously to assess metastatic spread.
Five-Year Survival Rates after Radical Hysterectomy
When lymph nodes remain untouched by cancer, survival statistics are extremely encouraging: 88% – 99% survival when pelvic lymph nodes are cancer-free.
However, if cancer has migrated into the pelvic lymph nodes, survival decreases significantly: 50% – 74% survival with pelvic lymph node involvement.
| Lymph node status | 5-year survival rate (post surgery) | Significance |
|---|---|---|
| Pelvic nodes negative | 88–90% | Extremely high cure rates, and surgery is often sufficient |
| Pelvic nodes positive | 50–74% | Decreased rates typically require adjuvant (postoperative) radiation and/or chemotherapy |
| Para aortic nodes positive | Significantly lower | This spread suggests more systemic disease; the outlook is more guarded, and survival approaches the lower end of the stage 3/4 spectrum |
The outlook becomes more guarded when para-aortic lymph nodes are affected. These nodes act like major highways for systemic spread; thus, cancer cells in this region suggest a more advanced biological behavior.
Effect of the Number of Affected Lymph Nodes
The extent of nodal involvement acts as a prognostic compass:
- 1 affected lymph node: $\sim 62%$ survival
- 2 affected lymph nodes: $\sim 36%$ survival
- 3–4 affected nodes: approximately $20%$ survival
- 5 or more nodes: survival approaches $0%$
These figures underscore the urgency of early detection and timely intervention, particularly in lower-resource regions where routine screening may be inconsistent.
Prognosis According To Cervical Cancer Stage
Once treatment adheres to established global protocols, whether in Europe, India, Turkey, Southeast Asia, or South America, the likelihood of long-term survival significantly improves. Across international oncology centers, the five-year survival spectrum ranges widely depending on stage:
Five-Year Survival Rate by Stage
Stage I: 85% – 90%
Cancer confined to the cervix.Stage II: 70% – 75%
Cancer has spread beyond the uterus to nearby areas like the upper vagina, but not to the pelvic wall or lower third of the vagina.Stage III: 30% – 35%
Cancer has spread to the pelvic side wall, involves the lower third of the vagina, or can affect the kidney (hydronephrosis).Stage IV: 5% – 7%
Cancer spreads to distant organs; metastasis to lungs, liver, bone, or involves the bladder or rectal tissues.
The past decade has witnessed meaningful improvements in survival among early-stage patients, largely due to advances in robotic surgery, targeted radiation therapy, improved pathology assessment, vaccination programs, and earlier detection through HPV testing.
Risk of Recurrence after Treatment
Cervical cancer’s recurrence profile requires careful long-term monitoring. Recurrence means the cancer has resurfaced after a period of remission, often because a cluster of microscopic cancer cells survived initial therapy and later multiplied.
Patterns and Timing of Recurrence
- 70%–75% of relapses occur within the first 3 years after treatment.
- Recurrence hot spots include:
- Vagina: $40%–45%$
- Pelvic lymph nodes: $25%–30%$
- Distant metastasis: $25%–30%$ (lungs, liver, bones)
The earlier a recurrence is detected, the better the odds of achieving a meaningful response to treatment.
Treatment Success in Recurrent Disease
Pelvic radiation therapy offers renewed hope for about $25%$ of women experiencing local recurrence. Once distant metastasis occurs, the probability of a favorable response drops to around $10%$.
Newer treatments like immunotherapy, targeted biological drugs, and proton therapy continue to redefine recurrence management, giving patients more options than ever before.
Life after Cervical Cancer Treatment
The conclusion of treatment does not immediately equate to the end of physical, emotional, or hormonal challenges. Many women describe their recovery journey as a long, unwinding path rather than a single definitive endpoint.
Long-Term Quality-of-Life Impact
Multiple studies have assessed how cervical cancer survivors live years after treatment. In one significant study of 120 women with early-stage cancer, none experienced recurrence over seven years, but many faced lingering symptoms such as:
- Chronic pelvic discomfort
- Fatigue or toxic-metabolic sensations
- Urinary difficulties
- Intestinal irregularities
- Shifts in sexual function
Another cohort of 98 long-term survivors reported challenges persisting 5 to 15 years after surgery, underscoring the importance of supportive care.
Radiation and Surgical After-Effects
Radiation therapy, though lifesaving, may affect:
- Soft tissue elasticity
- Vaginal lubrication
- Pelvic nerve sensitivity
- Bladder and bowel habits
Many patients describe the changes as subtle yet persistent echoes of treatment that occasionally resurface long after the cancer is gone.
Reproductive and Hormonal Considerations
Cervical cancer treatment intersects deeply with reproductive identity, especially because $40%$ of patients are under age 45. Many women facing this diagnosis still hope for future pregnancies, making fertility preservation an integral part of pre-treatment counseling.
How Treatment Impacts Fertility
- Radical hysterectomy removes the uterus but often leaves the ovaries intact. However, surgical disruption of the blood supply may eventually affect ovarian function.
- Radiation therapy can impair ovarian follicles, sometimes leading to premature ovarian insufficiency.
- Chemotherapy may also cause temporary or permanent changes in menstrual patterns.
For patients wanting to preserve fertility, doctors may recommend:
- Ovarian transposition (moving ovaries out of radiation fields)
- Cryopreservation of eggs or embryos
- Fertility-sparing surgery (trachelectomy) in select early-stage cases
Managing Treatment-Induced Menopause
When menopause occurs prematurely due to treatment, hormone replacement therapy (HRT) often becomes essential, especially for younger women. HRT can ease:
- Vaginal dryness
- Hot flashes
- Painful intimacy
- Mood fluctuation
The goal is to restore a sense of normalcy and maintain bone and cardiovascular health.
Changes in Sexual Health after Treatment
Treatment for cervical cancer may reshape the anatomy and physiology of the pelvic region, influencing intimacy. Many women worry about sexual function after surgery or radiation; fear, pain, and psychological stress frequently intertwine.
Common Post-Treatment Sexual Concerns
Doctors have observed consistent patterns across multiple studies:
- Women who received radiation after surgery faced more intense sexual side effects than those treated with surgery alone.
- Survivors who avoided adjuvant chemotherapy often reported sexual well-being similar to that of healthy women.
- The most prevalent concern was reduced lubrication, not loss of desire.
- Orgasmic function generally remained intact, although anxiety sometimes affected responsiveness.
- Pain during intercourse was common for up to 3 months post-surgery and could last up to 2 years after radiation therapy.
Tools That Help
Managing intimacy-related symptoms often requires a combination of:
- Medical lubricants
- Vaginal moisturizers
- Local estrogen therapies
- Pelvic-floor rehabilitation
- Counseling focused on sexual confidence
Patients often recover far better when these concerns are addressed early rather than left unspoken.
Holistic Recovery and Emotional Healing
Cancer, even when medically cured, can leave psychological imprints. Survivors often describe feelings that oscillate between triumph and vulnerability. Many medical tourism programs now integrate supportive services such as:
- Psycho-oncology counseling
- Survivorship workshops
- Nutritional rehabilitation
- Yoga and pelvic physiotherapy
- Mindfulness-based stress reduction
These modalities help patients rebuild not just physically but emotionally, rediscovering pleasure, confidence, and autonomy.
Fertility Preservation: The Radical Trachelectomy Success Story
For many patients under 45 (who represent roughly $40%$ of cases), preserving the ability to carry a child is paramount. The gold-standard fertility-sparing surgery for highly selected early-stage cervical cancer is the Radical Trachelectomy (RT).
Oncologic and Reproductive Outcomes of Radical Trachelectomy
Clinical data, including large case series, have validated the safety and efficacy of RT, showing that for the right patient, it does not compromise survival:
- Oncologic Success: The 5-year overall survival and recurrence-free survival rates after RT (both vaginal and abdominal) are consistently reported as being equivalent to those after radical hysterectomy.
- Recurrence: The recurrence rate is low, with recurrence most likely occurring within the first few years.
- Pregnancy Rate: The reported post-trachelectomy pregnancy rate ranges, but large systematic reviews show a pooled pregnancy rate of $24%$ for women attempting conception, with a live birth rate of approximately $75%$ of those pregnancies.
The Main Challenge: The removal of the cervix (and replacement with a stabilizing cerclage) significantly increases the risk of preterm delivery and later miscarriage. This requires close monitoring by a high-risk obstetrics team.
The Evolving Landscape of Recurrent Disease: Immunotherapy
While recurrence significantly lowers the likelihood of a cure, newer systemic treatments have drastically changed the management of recurrent or metastatic (Stage IV) cervical cancer.
The Mechanism of Immune Checkpoint Inhibitors (ICIs)
Cervical cancer is caused by the Human Papillomavirus (HPV), making the resulting tumors highly visible to the immune system. However, cancer cells use "immune checkpoints" like the PD-1/PD-L1 axis as a cloaking mechanism to hide from immune T-cells.
- How it Works: Immunotherapy drugs, specifically Immune Checkpoint Inhibitors (ICIs) like pembrolizumab (Keytruda), block this "stop signal." This effectively takes the brakes off the T-cells, allowing them to recognize and attack the cancer.
- Current Standard of Care: ICIs combined with chemotherapy (and sometimes bevacizumab) are now the standard first-line treatment for many women with recurrent or metastatic cervical cancer, significantly improving overall survival and progression-free survival compared to chemotherapy alone.
Life After Cancer: The Long Road of Survivorship Quality of Life
Long-term survivors, though cured of cancer, often deal with persistent side effects of treatment. This is not just about physical symptoms; it includes mental and emotional health.
Persistent Symptoms for Long-Term Survivors
Research shows that while global quality of life scores tend to be "good" for survivors, specific domains remain problematic, often tied to the intensity of treatment (especially radiation):
- Sexual Dysfunction: Consistently reported as the domain with the lowest scores across multiple studies, including issues with pain (dyspareunia), reduced enjoyment, and sexual worry.
- Lymphedema: Chronic swelling, often in the legs or groin, resulting from the surgical removal and/or radiation of lymph nodes. Lymphedema requires lifelong management with physical therapy and compression.
- Gastrointestinal and Urogenital Issues: Changes to bowel and bladder function (constipation, diarrhea, urgency) due to radiation's effect on the nearby organs.
- Mental Health: Cervical cancer survivors report higher rates of depression and anxiety compared to the general population, emphasizing the need for robust psycho-oncology support.
The Survivorship Plan
A holistic recovery plan must involve:
- Pelvic Floor Rehabilitation: Essential for managing urinary, bowel, and sexual side effects.
- Hormone Restoration: Proactive HRT management for treatment-induced menopause.
- Psycho-Social Support: Integration of counseling, mindfulness, and support groups to rebuild emotional health and body confidence.
Why Early Detection Holds Extraordinary Power
Cervical cancer is one of the few malignancies with a highly preventable trajectory. A combination of HPV vaccination, routine Pap smears, and HPV DNA testing can identify abnormal changes years before they evolve into cancer.
Countries with high screening coverage report dramatic drops in incidence and improved survival outcomes. This is precisely why many women travel internationally for advanced diagnostic tools, robotic surgeries, proton therapy, and specialized gynecologic oncology services.
Human Papillomavirus Vaccine
The HPV vaccine is one of the most powerful tools in modern medicine, often referred to as an anti-cancer vaccine because it directly prevents the viral infection that causes the vast majority of cervical and various other cancers.
1. The Mechanism of Action
- Targeting High-Risk Types: The vaccine is a preventative shot that contains proteins resembling the outer coat of the high-risk HPV types, particularly HPV-16 and HPV-18, which cause about $70%$ of all cervical cancers.
- Immune Response: Because the vaccine does not contain actual viruses, it cannot cause an infection. Instead, it safely stimulates the body’s immune system to produce high levels of antibodies against these specific HPV types.
- Protection: If the person is later exposed to the virus, these antibodies recognize and quickly neutralize the HPV particles, preventing the infection from ever establishing itself. Since persistent infection with high-risk HPV is the cause of cervical cell changes that lead to cancer, blocking the infection prevents the cancer from starting.
2. Cancers Prevented by the HPV Vaccine
The vaccine protects against several HPV-related cancers, not just cervical cancer:
- Cervical Cancer
- Vaginal and Vulval Cancers
- Anal Cancer
- Penile Cancer
- Oropharyngeal (Mouth and Throat) Cancers
Efficacy and Cancer Prevention Statistics
| Study Location (Population) | Age at Vaccination | Reduction in Invasive Cervical Cancer |
|---|---|---|
| Sweden (1.7 million women) | Before age 17 | Nearly 90% reduction |
| Scotland (Long-term data) | Age 12–13 | No cases recorded in women vaccinated at this age |
| Netherlands (Bivalent vaccine) | Age 16 | Lowered risk by 92% |
Overall, Young Women (Pre-exposure) in Systematic Reviews have shown results of "Remarkably High" in preventing high-grade precancerous lesions (up to $98%$ for targeted HPV types). The younger the age at vaccination (before exposure), the greater the protection.
Indications and Recommended Ages
Global health authorities, including the CDC and WHO, recommend the HPV vaccine for both males and females.
Routine Vaccination (Optimal Age)
- Ages: 11 or 12 years (can be started as early as 9 years).
- Dosing Schedule (Ages 9–14): Two doses are recommended, usually given 6 to 12 months apart.
Catch-Up Vaccination
- Ages: 15 through 26 years (if not adequately vaccinated when younger).
- Dosing Schedule (Ages 15–26): Three doses are recommended, typically given at 0, 1–2 months, and 6 months.
Shared Clinical Decision-Making
- Ages: 27 through 45 years (Some adults in this age range may decide to get the HPV vaccine based on a discussion with their clinician).
Types of HPV vaccines
The HPV vaccines are categorized by the number of HPV types they protect against. Gardasil 9 is the most widely used and broadly protective vaccine currently available in most regions.
| Vaccine Type (Brand) | HPV types covered | Target cancer prevention | Age group |
|---|---|---|---|
| Nonavalent (Gardasil 9) | 9 types: HPV 6, 11, 16, 18, 31, 33, 45, 52, 58 | Covers 75-90% of cervical cancers and genital warts | 9 to 45 years |
| Quadrivalent (Gardasil 4, CERVAVAC) | 4 types: HPV 6,11,16,18 | Covers 70% of cervical cancers and genital warts | 9 to 26 years |
| Bivalent (Cervarix) | 2 types: 16,18 | Covers 70% cervical cancers (most prominent for cancer-causing strains) | 9 to 26 years |
The Importance of Screening (Even with Vaccination)
While the HPV vaccine is incredibly effective, it does not replace the need for regular cervical cancer screening (Pap smears and HPV testing). No vaccine offers $100%$ protection against all high-risk HPV strains, so screening remains the necessary safety net for detecting any abnormalities early.
Key Takeaways for International Patients Seeking Cervical Cancer Treatment
- Cervical cancer prognosis varies widely based on stage, lymph node involvement, and histological type.
- Early-stage disease treated with radical hysterectomy offers survival rates exceeding $85%$.
- Recurrence is most likely within 3 years; vigilant follow-up is essential.
- Fertility-sparing procedures (like Radical Trachelectomy) and hormonal therapies can help preserve reproductive and sexual wellness.
- Survivorship extends beyond cure; it involves holistic rehabilitation and psychological restoration.
For many women, seeking treatment abroad unlocks access to cutting-edge technologies, skilled surgical teams, and compassionate long-term support programs that are essential for regaining a sense of wholeness after cancer.