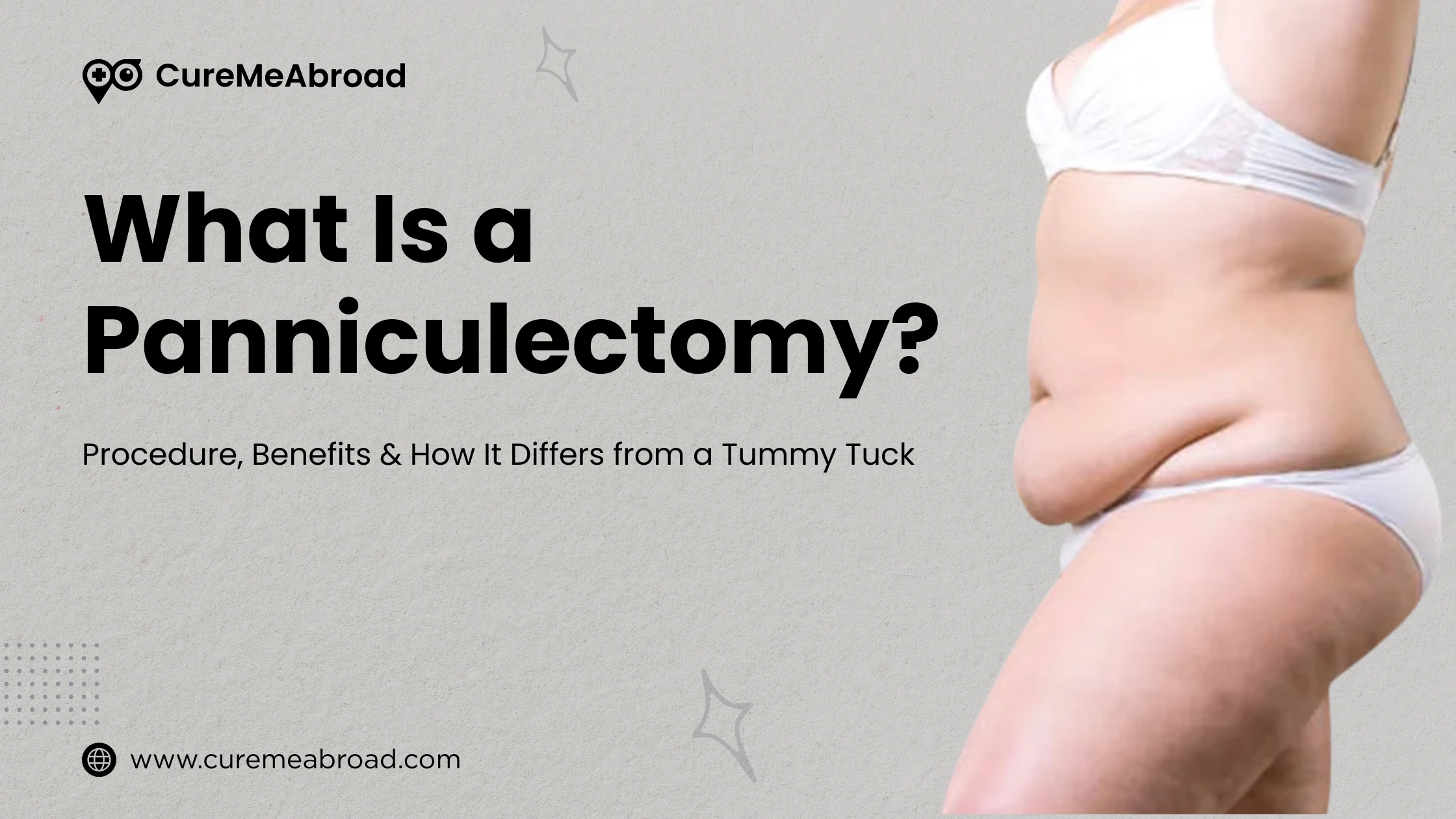
What is a Panniculectomy?
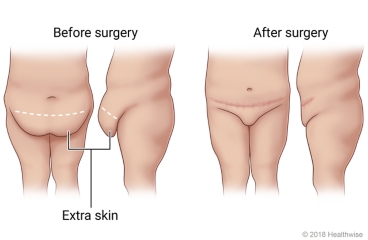
The “pannus” is an apron of skin that hangs down over the stomach, legs, and genitals following a massive weight loss. A panniculectomy is a surgical body contouring procedure that removes this loose, sagging skin from the abdomen and surrounding regions.
Why the Procedure Is Performed
Significant weight loss often following bariatric surgery or lifestyle changes can result in loose, hanging folds of skin that no longer retract due to a loss of elasticity. This excess skin can cover the thighs and genitals, leading to discomfort, hygiene issues, skin irritation, and challenges with daily activities. It can also cause rashes and sores, making it difficult to find well-fitting clothing.
A panniculectomy helps eliminate this extra tissue, enhancing both comfort and appearance. Patients frequently report feeling lighter, more confident, and relieved from ongoing skin infections or irritation after the pannus is removed.
WHAT TO EXPECT BEFORE, DURING AND AFTER THE SURGERY?
A panniculectomy is usually carried out in a hospital or surgical center and can take several hours to finish. The procedure is performed under general anesthesia, ensuring that you remain asleep and free from pain throughout.
During the surgery, the surgeon creates an incision typically a horizontal one just above the pubic area, extending till the belly button, depending on how much tissue needs to be removed. The overhanging skin and fat, referred to as the pannus or "apron," are carefully excised. After removing the excess tissue, the incision is closed with sutures, and small drainage tubes may be inserted to assist in draining any excess fluid as the area heals. A sterile dressing and sometimes an abdominal binder are applied to support the healing tissues and minimize swelling.
Risks and Possible Complications
Like any significant surgery, a panniculectomy comes with certain risks related to anesthesia and the procedure itself. These risks include:
- Allergic reactions to medications
- Breathing difficulties
- Bleeding, infection, or blood clots
There are also specific risks linked to panniculectomy, such as:
- Noticeable scarring
- Nerve injury or temporary numbness
- Fluid accumulation (seroma)
- Poor wound healing or tissue death
- Ongoing looseness of the skin
Your surgeon will thoroughly discuss these risks with you before the procedure and provide guidance on how to minimize them.
Preparing for the Surgery
Before your surgery, your surgeon will review your medical history in detail, examine any excess skin, and evaluate any previous scars. Be sure to inform your medical team if you are pregnant, could be pregnant, or if you're taking any prescription medications, supplements, or herbal products.
About a week before the procedure, you need to stop taking blood-thinning medication like aspirin, ibuprofen, naproxen, vitamin E, or specific prescription drugs to decrease the risk of bleeding. On the day of the surgery, be sure to follow all fasting guidelines and take only approved medications with a small sip of water.
After the Surgery
Most patients stay in the hospital for about two days after surgery, though more complex cases might require a longer hospitalization. Once you are fully awake, you'll be encouraged to walk short distances to promote circulation and reduce the risk of blood clots.
During the initial recovery phase, it's common to experience pain, swelling, bruising, and numbness. Your surgeon will prescribe pain medication and recommend that you rest with your knees and hips slightly bent to alleviate abdominal tension. Within a day or two after surgery, you'll start wearing an elastic compression garment or binder for support and to help minimize swelling.
For at least 4–6 weeks, avoid strenuous activities and heavy lifting. Plan on returning to work around 4 weeks, depending on how comfortable you feel. While most swelling will subside within 3 months, complete healing including scar softening and achieving final contour results can take up to 2 years.
BENEFITS OF PANNICULECTOMY
- Improved skin health and hygiene: Due to loose skin it becomes difficult to wash and maintain hygiene in sweaty areas like inner thighs, below the belly, and genitals. This often leads to rashes in these areas and harbors bacteria. Panniculectomy helps with this and prevents the risk of infection.
- Helps in better movement and easy daily activities Patients experience ease in walking, exercising, and performing their daily tasks.
- Reduced back pain and improvement in overall well-being of the patient
- Patients often benefit from the improved appearance, which helps their emotional and mental well-being.
HOW IS IT DIFFERENT FROM TUMMY TUCK?
- Panniculectomy specifically removes excess hanging skin from the abdomen while a tummy tuck (abdominoplasty) is more of a cosmetic procedure.
- Surgical scope: A tummy tuck also focuses on abdominal tightening and contouring, while panniculectomy focuses on skin removal.
- Candidates: Panniculectomy is for patients who had massive weight loss but don’t have issues with their abdominal muscles. A tummy tuck is for patients who want to improve their abdominal contour and tightening.